Beyond Charlie Sheen’s Claim: The Real Story Behind the ‘Suppressed’ HIV Drug

Sarah Johnson
December 12, 2025
Brief
Charlie Sheen’s claim about a “suppressed” HIV drug taps into deep distrust of Big Pharma. This analysis unpacks the real leronlimab story, HIV history, and the politics of medical innovation.
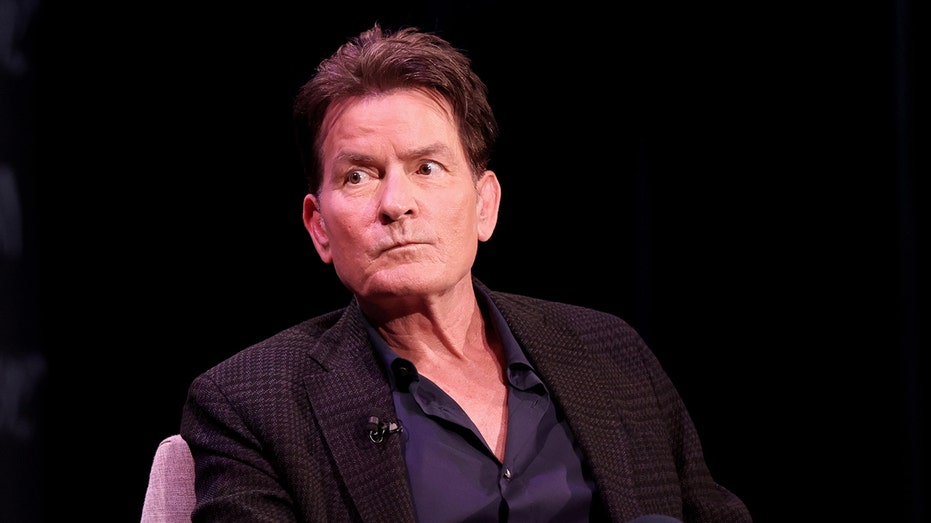
Charlie Sheen, the ‘Suppressed’ HIV Drug, and the Bigger Story About Trust in Medicine
When Charlie Sheen claims an experimental HIV treatment was kept off the market because it was “a threat” to the industry, he’s doing more than revisiting his own health history. He’s tapping into a powerful and growing public narrative: that life-saving medical innovations are routinely buried to protect profits. Whether his specific allegation holds up or not, the controversy around PRO 140 — now known as leronlimab — exposes deep tensions at the intersection of celebrity, science, regulation and distrust of Big Pharma.
To understand why this comment resonated so widely, we need to look far beyond one actor’s podcast interview and examine the real, complicated history of HIV treatment, biotech failures, regulatory hurdles, and the collapse of public confidence in medical institutions.
From Death Sentence to Chronic Condition: Why Alternatives Like PRO 140 Appealed
Sheen’s suggestion that PRO 140 delivered “quicker and more stable results with no side effects” than traditional HIV therapy speaks to a real and longstanding problem: even though modern antiretroviral therapy (ART) is extraordinarily effective, it’s often far from easy.
- In the mid-1990s, combination ART turned HIV from a near-certain death sentence into a manageable chronic disease. AIDS deaths in the U.S. fell by roughly 60% between 1995 and 1998 as new drug cocktails rolled out.
- But treatment has come at a cost: lifelong daily pills, complex regimens, drug interactions, weight gain, metabolic issues, and long-term toxicities have been extensively documented in clinical literature.
- Even today, adherence is a major challenge. Studies consistently show that a significant portion of patients on ART struggle with missed doses, side effects, or treatment fatigue.
Enter monoclonal antibodies like PRO 140/leronlimab. Instead of targeting the virus directly, leronlimab targets CCR5, a receptor on immune cells that many HIV strains use to enter the cell. It has been studied as a once-weekly subcutaneous injection, and early research suggested it could maintain viral suppression in some patients with fewer systemic side effects.
To a patient exhausted by pills, side effects, and stigma, the promise of a weekly injection with a different safety profile is compelling. Sheen’s praise of the drug is consistent with how many trial participants describe novel therapies that temporarily liberate them from the rituals and reminders of chronic illness.
Leronlimab’s Real Story: Not a Conspiracy, But a Cautionary Tale
Sheen frames the drug’s failure to launch as an act of suppression: “It’s a threat, I suppose… It works, better than what they have.” The public hears this and immediately slots it into a familiar narrative of corporate sabotage. But the actual history of PRO 140/leronlimab paints a more complicated picture.
Publicly available regulatory and corporate records show a story less about a miracle drug killed by competitors and more about a small biotech company overpromising, under-delivering, and running into regulatory and financial trouble.
- Leronlimab has been in development for years and has gone through multiple phases of clinical trials for HIV and, later, COVID-19 and cancer indications.
- The U.S. Food and Drug Administration (FDA) repeatedly raised concerns about the quality of the clinical data, trial conduct, and the sponsor’s regulatory submissions. At several points the agency issued rebukes over inadequate or incomplete information.
- The company behind leronlimab became embroiled in SEC investigations, lawsuits, and management turnover, with critics accusing it of hyping preliminary findings to investors and the public.
This isn’t the profile of a clean, well-run program that was crushed by a jealous pharmaceutical giant. It looks more like a classic small biotech overreach: an interesting molecule, intriguing early data, but shaky corporate governance and patchy evidence. That doesn’t prove leronlimab has no therapeutic value; it does show why regulators remain unconvinced.
In other words, there’s a difference between “this drug was suppressed” and “this drug didn’t meet the evidentiary standards needed for approval, at least so far.” That nuance often disappears when a celebrity collapses a long, messy history into a single soundbite.
Why the ‘Suppressed Cure’ Narrative Is So Powerful Right Now
Sheen’s comments land in a climate where trust in pharmaceutical companies and health regulators is historically fragile. Multiple trends collide here:
- Decades of Big Pharma scandals. From opioid marketing that fueled addiction epidemics to insulin price spikes, the industry has repeatedly demonstrated that profit can trump patient welfare. This primes the public to believe that any non-commercialized breakthrough must have been buried for financial reasons.
- COVID-19-era information wars. Public debates over vaccines, therapeutics, mask mandates, and emergency approvals have left many people convinced that regulators are either captured by industry or actively hiding information.
- Social media amplification. A remark made casually on a podcast can instantly circulate through communities already predisposed to distrust official narratives. The story becomes evidence for pre-existing beliefs, not a starting point for investigation.
- HIV’s own history of activism. In the 1980s and 1990s, HIV activists correctly accused regulators and drug companies of moving too slowly, and of ignoring patients’ voices. That legacy of justified anger now coexists with a heavily commercialized treatment landscape.
Against this backdrop, Sheen’s assertion feels plausible to many, even if the documented record points to a more mundane explanation: scientific uncertainty and corporate dysfunction.
Celebrity, Stigma, and the Politics of HIV Narratives
Sheen is not just any patient; he is one of the few high-profile Hollywood figures to publicly disclose his HIV status. His story—addiction, sexual risk-taking, blackmail, and eventual control of the virus—touches almost every sensitive nerve in the public imagination about HIV.
Historically, celebrities with HIV have had outsized influence on how the disease is understood:
- Rock Hudson’s death in 1985 forced mainstream America to confront AIDS.
- Magic Johnson’s 1991 announcement helped destigmatize HIV and demonstrated that a long life with the virus was possible.
- Freddie Mercury’s death centered the epidemic in global pop culture.
Each of these figures shifted public discourse toward empathy and away from moral judgment, albeit slowly. Sheen’s narrative does something more paradoxical: it both humanizes HIV (by speaking frankly about addiction, sex with men, and survival) and feeds skepticism about the medical system sustaining his life.
That tension is critical. On the one hand, Sheen openly describes the relief of knowing there was a “discipline of high-tech medicine” ready to “drive [HIV] into submission.” On the other, he portrays that same system as potentially blocking better options. This ambivalence mirrors a broader cultural mood: dependence on science, combined with deep suspicion of the institutions that deliver it.
Are We Overlooking Structural Problems Behind the Conspiracy Talk?
Focusing on whether one drug was “kept off the market” risks missing more systemic failures that make such allegations resonate:
- Perverse incentives in drug development. Investors often demand short-term gains, pushing small biotechs to oversell early data. This increases the chances that promising molecules will be mismanaged, not maximized.
- Regulatory opacity. While the FDA publishes some documents, much of the back-and-forth with companies remains opaque to the public. In that vacuum, conspiracy theories flourish.
- Access and equity issues. For many people living with HIV—especially in low- and middle-income countries—the idea of a once-weekly, low-side-effect injection is tantalizing because existing treatments, even if effective, are hard to access or maintain.
- Stigma and mental health. Sheen’s description of the psychological relief after diagnosis underscores how HIV is as much a social and emotional condition as a biological one. A therapy that feels less stigmatizing—fewer visible pill bottles, fewer daily reminders—can be life-changing even if it’s only marginally superior clinically.
These structural issues don’t require a conspiracy to explain why some innovations stumble or vanish. They do, however, explain why people easily believe that the system doesn’t always act in patients’ best interests.
Expert Perspectives: Between Hope and Hype
In conversations with HIV researchers and bioethicists, a common theme emerges: drugs like leronlimab represent genuine scientific creativity, but they must be judged by data, not anecdotes—no matter how famous the patient.
HIV specialists point out that the current standard of care—integrase inhibitor–based regimens, often as a single daily tablet—achieve viral suppression in over 90% of adherent patients with relatively mild side effects compared to earlier eras. For a new drug to replace or supplement these regimens, it needs to show not just promise, but clear, reproducible superiority or a special niche (such as salvage therapy for highly resistant virus, or a major adherence advantage).
Bioethicists, meanwhile, warn that celebrity endorsements of experimental therapies can distort both public perception and patient expectations. When a well-known figure describes a trial drug as dramatically better, others may pressure their physicians for access or become disillusioned when they can’t get it, even though the evidence remains preliminary.
What This Means for Patients, Regulators, and the Industry
The Sheen–PRO 140 story carries several implications that extend beyond HIV:
- For patients: It underscores the importance—and the challenge—of navigating between hope and evidence. Experimental therapies can be transformative for some individuals, but personal experience is not a substitute for large, rigorous trials.
- For regulators: The episode highlights how poor transparency can feed suspicion. Making more of the regulatory reasoning, data critiques, and trial shortcomings accessible in plain language could help counter “suppressed cure” narratives.
- For industry: Biotech companies that oversell early-stage drugs and under-deliver on data erode trust not only in themselves but in the entire innovation ecosystem. The line between legitimate optimism and hype is thin, but crossing it has real public health costs.
- For media: Entertainment interviews with celebrities about health issues can easily slide into unchallenged claims. Without context, a remark about an “industry threat” can harden into “proof” for millions of listeners already primed to distrust medicine.
Looking Ahead: How Stories Like This Will Shape the Next Phase of HIV Care
HIV medicine is entering a new phase. Long-acting injectable regimens are already being used; implants and even gene-editing strategies are under study. In that context, leronlimab is neither a miracle cure nor a meaningless dead end—it’s part of a broader wave of attempts to make HIV treatment less burdensome and more personalized.
The critical question is not whether one drug was unjustly sidelined. It’s how the system can:
- Foster innovation in modalities beyond daily oral pills,
- Ensure that new therapies are evaluated rigorously and transparently, and
- Communicate both successes and failures in ways that earn, rather than erode, public trust.
As new long-acting and biologic therapies compete for approval and reimbursement, stories like Sheen’s will shape patient expectations and political pressure. Regulators and industry leaders ignore this narrative terrain at their peril.
The Bottom Line
Charlie Sheen’s allegation that an HIV drug was kept off the market because it threatened the industry encapsulates a deeper crisis of confidence in modern medicine. The documented history of PRO 140/leronlimab points more to scientific and corporate shortcomings than to a coordinated effort to bury a breakthrough. But in a world of expensive drugs, opaque regulation, and real past abuses by pharmaceutical companies, it’s not surprising that many people find the “suppressed cure” story more believable than the messy, less cinematic truth.
The challenge now is to build a medical system—and a communication culture—where patients don’t have to choose between blind trust and blanket suspicion. That will require not just better drugs, but better data, better transparency, and a far more honest conversation about how health innovation actually works.
Topics
Editor's Comments
What’s striking about the Sheen–PRO 140 story is how little oxygen the actual science and regulatory record receive compared with the celebrity anecdote. In many ways, leronlimab is a case study in how structural weaknesses in the biomedical innovation system get rhetorically converted into conspiracy. A small company arguably overpromised, under‑delivered, and then collided with a regulator that struggles to communicate its reasoning in a way laypeople can understand. That vacuum is filled by a simple story—industry kills miracle drug—which is emotionally powerful precisely because it echoes real historical abuses. The more unsettling question is not whether one HIV drug was suppressed, but whether our current model of drug development—dependent on speculative capital, opaque review processes, and marketing‑driven narratives—virtually guarantees periodic eruptions of this kind of distrust. Until we address those underlying incentives and communication failures, every high‑profile non‑approval will be a fresh opportunity for the ‘suppressed cure’ narrative to grow.
Like this article? Share it with your friends!
If you find this article interesting, feel free to share it with your friends!
Thank you for your support! Sharing is the greatest encouragement for us.