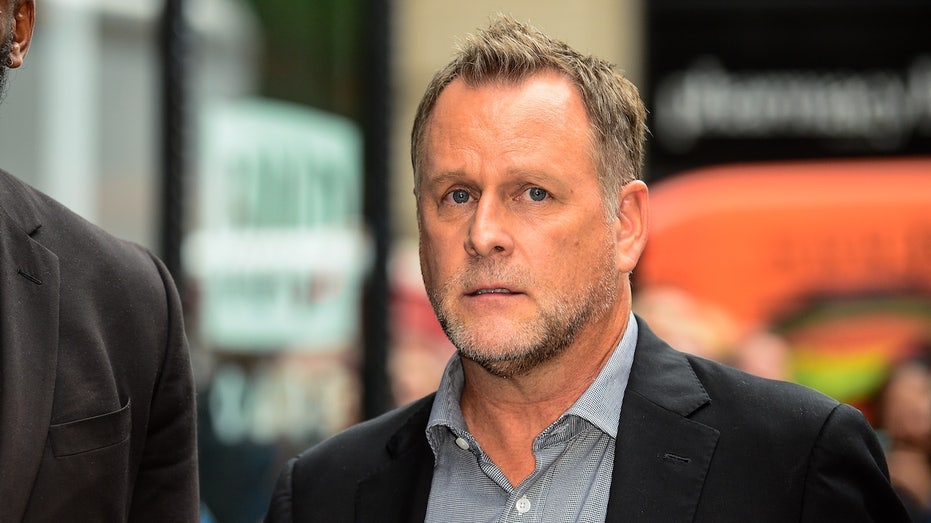
Dave Coulier’s Second Cancer Diagnosis Exposes Complex Challenges in Survivorship and HPV-Driven Malignancies

Sarah Johnson
December 3, 2025
Brief
Dave Coulier's second cancer diagnosis underlines critical issues in cancer survivorship, HPV-related cancer risks, and the need for vigilant monitoring and awareness among survivors and healthcare providers.
Opening Analysis
Dave Coulier's confronting a second, distinct cancer diagnosis less than a year after beating non-Hodgkin lymphoma reveals more than a personal health battle—it sheds light on the complex interplay of cancer survivorship, viral oncology, and the evolving medical landscape detecting multiple primary cancers. His case highlights both advances in early detection and the persistent vulnerabilities survivors face, especially from HPV-driven malignancies.
The Bigger Picture
Cancer survivorship has improved markedly over recent decades due to advances in treatment modalities such as targeted chemotherapy and radiation therapy. However, the emergence of multiple primary cancers in survivors is an increasingly recognized phenomenon. Historically, cancer survivors were primarily concerned with recurrence of their initial tumor, but growing data shows a notable risk for distinct new cancers potentially linked to shared risk factors or treatment effects.
HPV-related oropharyngeal cancers have soared in incidence since the early 2000s, now representing a majority of oropharyngeal carcinomas in the U.S. The human papillomavirus (HPV), especially HPV-16, is a known etiologic agent in these cancers, which often develop decades after initial infection. This latency, coupled with the widespread prevalence of HPV, presents challenges in screening and prevention.
Meanwhile, non-Hodgkin lymphoma (NHL) remains one of the most common hematologic cancers in adults. Treatments often include chemotherapy agents that can compromise immune function and influence secondary cancer risk.
What This Really Means
Coulier's new diagnosis of a P16-positive, HPV-related carcinoma shortly after remission from NHL encapsulates the multifactorial cancer risks survivors face. It reflects the potential for viral oncogenesis to manifest clinically many years after initial infection. The delayed activation of HPV-related cancer pathways underscores a crucial aspect of survivorship care—ongoing vigilance beyond the timeline of the first cancer.
Furthermore, it illustrates how cancer therapies and their immunosuppressive side effects may interplay with viral latency and immune surveillance failures, facilitating new malignancies. This second diagnosis also highlights the importance of advanced imaging like PET scans in detecting early, otherwise asymptomatic cancers, which can dramatically improve prognosis when caught timely.
Coulier’s openness about his experience also reduces stigma and raises awareness around cancers associated with HPV infection, oftentimes overshadowed by cervical cancer conversations and less familiar to the public when occurring in the oropharynx.
Expert Perspectives
Dr. Elizabeth Tran, Oncologist and HPV Cancer Researcher: "Dave Coulier’s case is emblematic of the long latency period characteristic of HPV-related cancers. It emphasizes the need for awareness that these malignancies can appear decades after initial viral exposure. Early detection through vigilant surveillance, especially in cancer survivors, is vital for high cure rates."
Dr. Michael Reynolds, Hematologist specializing in Lymphoma: "Non-Hodgkin lymphoma treatment can temporarily diminish immune function, which may potentially allow dormant viral infections like HPV to manifest clinically. This interplay merits further investigation to optimize follow-up care for survivors to balance cure with secondary cancer prevention."
Dr. Anita Shah, Epidemiologist at Cancer Prevention Institute: "The rising incidence of HPV-driven oropharyngeal cancers represents a significant shift in head and neck oncology. Coupling vaccination, education, and improved screening techniques could reduce this burden dramatically in the coming decades."
Data & Evidence
- HPV-related oropharyngeal cancers have increased over 225% since the early 2000s in the U.S., now comprising over 70% of such cancers.
- P16 positivity is a surrogate biomarker for HPV-driven cancers and is associated with better prognosis, with cure rates as high as 90% for early-stage disease.
- A 2019 National Cancer Institute study found cancer survivors have a 14% higher likelihood of developing a second primary malignancy compared to the general population.
- Non-Hodgkin lymphoma treatment protocols, including immunochemotherapy, are linked to long-term immunosuppression risks that may contribute to secondary cancer emergence.
- According to CDC data, HPV prevalence is estimated at 42.5% among American adults aged 18-59, underscoring the virus’s ubiquity but variable oncogenic potential.
Looking Ahead
Coulier’s journey underscores several future considerations in oncology and survivorship care:
- Enhanced surveillance protocols: Integrating viral biomarker testing and imaging follow-ups for survivors could enable earlier detection of secondary malignancies.
- HPV vaccination expansion: Increasing vaccination rates beyond young populations may help reduce the reservoir of latent infections contributing to adult cancers.
- Research into treatment interactions: Delineating how lymphoma therapies modulate viral oncogenic activation could guide tailored post-treatment monitoring and preventive interventions.
- Holistic survivorship care: Addressing psychological, nutritional, and lifestyle factors—as Coulier has through wellness initiatives—may improve overall resilience against recurrence or new cancers.
- Public awareness campaigns: Increasing understanding of HPV’s role in cancers beyond cervical cancer is essential to destigmatize and encourage screening and prevention efforts.
The Bottom Line
Dave Coulier’s dual cancer diagnoses illuminate the evolving realities of cancer survivorship, viral oncology, and the critical importance of vigilant, multi-pronged follow-up care. His experience spotlights how HPV-driven cancers can emerge decades after infection and how modern diagnostic tools can detect these early enough for highly effective treatment. It also raises vital questions about optimizing cancer survivor monitoring to prevent or rapidly address new malignancies, emphasizing an integrative approach to long-term health beyond initial remission.
Topics
Editor's Comments
Dave Coulier’s case vividly demonstrates the layered challenges facing today’s cancer survivors, particularly as we observe shifting cancer epidemiology toward virus-driven malignancies. It underlines an urgent need to rethink how survivorship care is structured—moving beyond monitoring just recurrence to anticipating and preventing second primary cancers that can emerge due to complex biological and treatment-related factors. Moreover, his openness helps break down stigma around HPV in non-cervical cancers, an important public health hurdle. As HPV vaccination campaigns have traditionally targeted younger populations, there is growing recognition that adult survivors and older demographics still face risks that call for innovative screening and education strategies.
Like this article? Share it with your friends!
If you find this article interesting, feel free to share it with your friends!
Thank you for your support! Sharing is the greatest encouragement for us.